- Metformin is commonly used in the treatment of diabetes.
- Metformin is structurally and chemically related to arginine, guanine and Canavanine.
- Side effects of Metformin include GI upset and autoimmune lupus (same with Canavanine.)
- Metformin also kills bacteria, i.e. it is an antibiotic.
- Many pharmaceuticals, e.g. statins, were first identified as antibiotics produced by fungi.
- Antibiotics select for antibiotic resistance genes, i.e. essential bacterial genes that have mutated to no longer be inactivated by antibiotics.
- New antibiotic resistance genes are combined with other resistance genes on multiple resistance plasmids that are transferred as a group.
- Because of its wide use, resistance to Metformin (and statins) as an antibiotic probably already exists and has been incorporated into multiple drug resistance plasmids.
- Many common pharmaceuticals are also antibiotics and probably select for multiple drug resistance.
- A major contributor to multiple drug resistance, “super bugs”, and the rapid loss of efficacy of antibiotics is the over use of pharmaceuticals in general, in addition to the specific abuse of antibiotics designed to kill pathogens.
Metformin is a Good Anti-Diabetic, but...
 |
| Arginine |
Metformin is a Diguanide
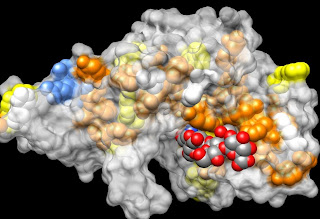
I previously explored the interesting properties of Metformin in my laboratory and through computer modeling experiments, and found it would react with many cellular enzymes and receptors similarly to the amino acid arginine. This was no surprise, since the working end of arginine is a guanide and Metformin is a Siamese twin of guanides, i.e. a biguanide. I might as well also say that another guanide, Canavanine, a toxic, antimicrobial phytoalexin in bean sprouts, has similar properties.
 |
| Canavanine |
Phytochemicals as Antibiotics
I have studied (and written about) the natural plant antibiotics, phytoalexins, in legumes, and particularly in soy beans, so I would expect all of the chemicals, (a.k.a. phytochemicals or “antioxidants”) extracted from plants, e.g. alkaloids, polyphenols and essential oils, to kill bacteria and be toxic to human cells. The selective advantage to plants in producing phytochemicals is the antibiotic activity of those chemicals. Pathogens that have adapted for growth on one species of plant have resistance genes to that plant’s phytoalexins. Thus, bacterial genes for resistance to the antibiotic activity of drugs derived from phytochemicals are common in nature and broad use of these drugs merely selects for the transfer of these genes to gut flora.
| Canavanine and Lupus What put together more pieces of the gut flora/antibiotic/autoimmune disease puzzle for me, was coming across Dr. Loren Cordain's recent reiteration of the toxicity of legumes and his singular example of Canavanine from alfalfa sprouts as a contributor to the autoimmune disease, lupus. When I looked up the structure of Canavanine and found it to be a guanide, I immediately started making comparisons to Metformin and was amazed to see that these chemicals share the same list of side effects focused on the gut. Moreover, lupus is also a side effect of both Metformin and Canavanine. It was initially surprising, that a recent study suggests that the anti-diabetic action of Metformin may result indirectly from its antibiotic effects on gut flora. I now expect that Canavanine causes lupus by killing or altering the metabolism of particular species of bacterial gut flora involved in the normal functions of the immune system, e.g. Tregs required for immune tolerance. It is now a common observation that many pharmaceuticals act indirectly via their impact on gut flora, i.e. many pharmaceuticals are fundamentally antibiotics, and particular antibiotics can duplicate the activity of pharmaceuticals. |
|